Pelvic floor dysfunction is often neglected and overlooked. Traditional chiropractic and physical therapy coursework lack appropriate education on the pelvic floor. Fortunately, an increasing number of pelvic floor-focused providers can help identify, treat, and manage pelvic floor dysfunction. I was lucky enough to sit down with pelvic floor expert, Kayla Ives, owner, and physical therapist at the Pelvic Physio Omaha.
The Pelvic Physio is the ONLY standalone pelvic floor clinic in Omaha, Nebraska. We recorded the video interview in her beautiful office complete with multiple treatment rooms, awesome natural lighting, a squat rack, and a living room that any daytime talk show would be jealous of.
You will learn from listening to the interview that Kayla takes a very global, holistic approach to the human body. Although she is a pelvic floor expert, she appreciates the complexity of the issues and conditions of the human body. One of her quotes that stuck out to me was,
“The pelvic floor is always the innocent bystander. Unless you have a direct scar, like from childbirth, it is normally not the pelvic floor’s fault you are having symptoms.”
Check out the full interview on our YouTube channel and be sure to keep reading for a dive into the questions and answers with some commentary from me!
What is the pelvic floor?

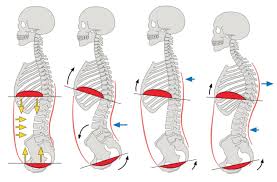
As simple as a group of muscles that are part of your core. It serves as the bottom of the core cannister. We’e discussed this core canister before and can be understood better with the soda can analogy.
A healthy core is like a soda can. It’s best to think of the core as an abdominal canister where the diaphragm is the top. The muscles between the rib cage and the pelvis are the sides and the bottom is the pelvic floor.
What is the function of the pelvic floor?
I first heard Kayla talk about the pelvic floor on a separate podcast. She was interviewed on the 4 M’s with Molly podcast and discussed the four main functions of the pelvic floor.
- Stability – the pelvic floor’s role in pain in the lower back, pelvis, sacroiliac joints, and hips.
- Sphincteric – stress urinary incontinence/leakage during exercise
- Sexual – role in penetration and orgasm.
- Support – Supports your organs like the Bladder, uterus, and rectum.
The two main functions of the pelvic floor we discussed in our interview were stability and sphincteric.
Myths and misconceptions about the pelvic floor
I think you can get a sense of Kayla’s sarcasm with the tunnel vision surrounding pelvic floor therapy. She highlights her global approach to pelvic floor treatment rather than dysfunction that needs to be trained individually with just a Kegel exercise.
She doesn’t completely disregard Kegel exercises, but in her experience, it is much more of a global problem not appropriately solved with a pelvic floor specific exercise.
What makes a healthy pelvic floor?
A healthy pelvic floor is an effective pressure management system. It relaxes with inhalation and contracts when you exhale. The pelvic floor issues that Kayla sees in the clinic are often the result of too much tension as compensation for ongoing weakness. She notes that nearly 95% of the people she sees have tension-related dysfunction.
“A healthy pelvic floor is a relaxed butthole.”
We had a good laugh about the relaxed butthole comment. I first heard her mentioned this on the podcast previously mentioned. She likes to use it as a cue to her patients to let go of all the tension they are holding in their pelvic floor. From a therapy standpoint, she teaches patients to relax their pelvic floor by breathing into a ball or their chair.
Stability function of the pelvic floor
The stability function of the pelvic floor is that it helps support the lumbar spine, pelvis, and hips by serving as the bottom of the core canister.
Kayla notes the stat that 80 percent of back pain suffers have pelvic floor dysfunction. She sees a pattern of too much tension in the hip rotators and a lack of appropriate glute max activation. Correcting this muscle imbalance between glutes and deep pelvic rotators is part of her approach to treating hip, pelvic, and lower back issues.
Sphincteric function of the pelvic floor

Urinary incontinence is extremely common in post-partum, athletic females with both lifting and running.
Kayla highlights that it is less about strength and more about pressure management and what happens in response to increases in intra-abdominal pressure. If someone goes to laugh, lift, or blow up a balloon and their pelvic floor goes down then it puts pressure on their bladder, and they are more likely to leak.
Getting the proper strategies to help better control pressure management is the most effective solution. She notes that oftentimes these improvements happen in the first six weeks, so we know it is not due to strength.
We briefly discuss whether powerlifters or runners with stress urinary incontinence/leakage are more difficult to rehab. Kayla believes that runners are typically harder to rehab given the complexity of some of their training and the difficulty to get them to scale or decrease their running.
To me, this seems counterintuitive. I personally don’t have a large enough sample size but given the higher intraabdominal pressures with competitive weightlifting, it would seem they would likely be more difficult to rehab for leakage with exercise.
More information can be found on the Barbell Medicine podcast by clicking here.
Post-partum pelvic floor health in vaginal versus Cesarean births
“It’s a different injury in a different area.”
Cesarean scars require more scar mobility but ultimately both are unique injuries that require different rehab because of the tissues involved.
I strongly encourage you to take the time to check out the full video on YouTube. It was fun to highlight Kayla’s expertise, and I look forward to future collaboration on difficult cases. Stay tuned for more interviews with local experts in our community.