The idea of a placebo is clearest to a parent of a young child. For example, Imagine your kid stumbles and scratches their knee. They run to you in tears and you console them, kissing their owie. Clearly, your kiss had no magical healing properties, but every parent can attest to how much it helps a child recover.
In general, the placebo effect is a phenomenon that occurs when an intervention improves a condition unexplained by the specific physiological effects. In other words, it is less about the actual intervention and more about the patient’s beliefs.
Check out this Ted Talk Video on Placebo:
What is a placebo?
The classic, placebo experiment is one in which two groups receive different pills. One group gets the real medication and another group receives a sugar pill. However, neither group is aware if they are taking the actual medication or the sugar pill. This type of research is known as a randomized placebo-controlled trial.
Research into the placebo effect is intriguing because it shows the power of the patient’s perception. In fact, many traditional treatments are no better than placebo, even surgery!
Certainly, chiropractic is an easy target. Admittedly, this is mostly self-inflicted. For example, some chiropractors continue to treat outside of their scope of practice, push the anti-vaccine agenda, and are just generally anti-medicine.
Why a false narrative?
First off, judging the effectiveness of treatment solely off the comparison to a placebo is reductionistic and fails to encompass a holistic view of health and treatment.
Many of the drugs and therapies that are ‘better than placebo’ have a small effect size. Meaning, the treatment groups are only slightly better than the placebo group. Even the most widely accepted truths in medicine often have a small effect size. For example, statins for heart disease are widely accepted as the best medication for the prevention of heart disease. However, for every 100 people who take a statin for the primary prevention of heart disease, only two will avoid a heart attack.
Placebo Surgery
In fact, some of the most common orthopedic surgeries are no better than placebo. For example, four of the most common orthopedic surgeries are no better than placebo for reducing patient’s pain and disability:
- vertebroplasty for osteoporotic compression fractures
- intradiscal electrothermal therapy for discogenic lower back pain
- arthroscopic debridement for osteoarthritis of the knee
- open debridement of common extensor tendons for tennis elbow
Specific Effect + Placebo
Every medical treatment has two components. The first being the specific effects of the treatment itself. The second being the knowledge that the treatment is being performed (the placebo effect). 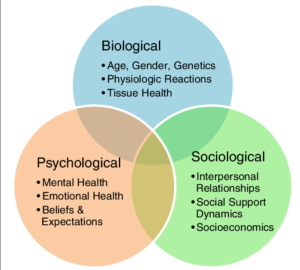
Ultimately, Pain is multi-factorial.
I think many people forget that patient’s are people rather than their conditions.
A healthy approach is understanding the bio-psycho-social model. This was discussed in a previous blog post: Treating Patients Not Pictures
Baby out with the bathwater
The context of the therapy matters. The interaction and rapport with your doctor matters. The placebo response is part of every intervention. It is the human component to taking care of people and it feels wrong to try to eliminate it. The doctor-patient interaction is not just this fluffy relationship to boost Google Reviews but boosts the effectiveness of treatment. Our focus should be on cultivating it. Developing better strategies for how doctors deliver treatment that takes into account patient values and communicating with them in a caring way. Research demonstrates:
Doctors who are warmer and more competent can set more powerful expectations about medical treatments. Those positive expectations, in turn, have a measurable impact on health.
I wrote a blog post about this a while back and it feels like the right time to reference it. The blog was based on an article in the NY Times: Can A Nice Doctor Make Treatments More Effective?
Not So Fast
There is still a lot of crap out there that works because an enthusiastic, snake-oil salesman peddles it. This article is not a call to disband evidence-based medicine. Rather, it is for evidence-based medicine to expand its view on why treatments work. I still believe in the importance of being evidence-based, treating within your scope of practice, and listening to the patient.
Take Home Points
- All treatments are composed of two things: Specific effects of treatment and the knowledge that treatment is being performed (placebo effect).
- Pain is complex, multifactorial: a biopsychosocial approach takes a more holistic view of health when compared to previous pathoanatomical thoughts.
- All medical treatments are subject to the placebo effect including surgery, medication, and chiropractic.
- Plenty of junk treatment out there – Avoid it and follow the science the best we can.